Stroke, once considered a condition of old age, is increasingly affecting younger people. What’s concerning is that most of them are unaware they’re even at risk.
According to Dr. Trần Quốc Tuấn, a neurosurgeon at the University Medical Center Ho Chi Minh City (UMC), this trend is not unique to Vietnam; it’s being seen worldwide. Stroke is now one of the leading causes of death and long-term disability, surpassing even heart disease in some cases.
Yet Dr. Tuấn also shares an encouraging statistic:
“The American Stroke Association estimates that up to 80% of strokes are preventable. That means young people can take steps to protect themselves, before it’s too late.”
There have been cases of young individuals experiencing strokes after activities like jogging, playing football, cycling, or working out,... all typically associated with good health. How do you explain this phenomenon?
The rise in stroke incidence among young adults is a growing global concern. Previously, stroke cases in individuals under 45 accounted for only about 5% in Europe and North America. Today, that figure has increased to 10-15%. This is no longer a localized trend, but a worldwide warning, and Vietnam is no exception.
What we’ve observed is that physical activity itself is not the cause of stroke. Rather, it can unmask underlying medical conditions that have gone undetected. Many young patients who experience a stroke have pre-existing risk factors that were either overlooked or not identified in time, often compounded by high levels of stress and unhealthy modern lifestyles.
These risk factors generally fall into three main categories:
- Traditional vascular risks, such as hypertension, diabetes, and dyslipidemia, which remain relevant regardless of age.
- Lifestyle-related risks that are more prevalent among younger individuals, including smoking (both traditional and e-cigarettes), excessive alcohol or caffeine intake, poor sleep hygiene, and diets high in fats, sugars, and processed foods. These habits contribute to metabolic imbalances and increased risk of thromboembolic events.
- Undiagnosed congenital or genetic conditions, which often remain silent until a stroke occurs. Some young patients may have asymptomatic congenital heart disease or connective tissue disorders that weaken vessel integrity. These are typically only discovered after a stroke, during diagnostic workups.
Additionally, vascular injury due to sudden or excessive physical exertion can also be a contributing factor. Intense movements, especially involving the neck, can sometimes lead to arterial dissection, which may result in an ischemic stroke.
In women, specific risk factors include pregnancy, due to significant physiological changes, and oral contraceptive use, particularly those containing estrogen. While the evidence remains subject to ongoing debate, studies have noted an increased risk of venous thromboembolism and ischemic stroke in certain high-risk populations.

Many people still mistake early signs of stroke, like dizziness or facial drooping, for what’s commonly known in Vietnamese folk medicine as “trúng gió” (catching a chill), and choose remedies like coin scraping or acupressure instead of going to the hospital. How can we tell the difference early on?
In traditional beliefs, “trúng gió” is often used to describe symptoms caused by sudden exposure to wind or cold weather. It typically refers to minor, non-specific ailments like fatigue or mild dizziness. Stroke, on the other hand, is a serious medical emergency that involves damage to the brain, either from a blocked artery (ischemic stroke) or bleeding in the brain (hemorrhagic stroke).
What often causes confusion is that both conditions may appear to affect consciousness; patients might feel drowsy or dazed. However, stroke almost always involves clear neurological deficits, meaning the person loses the ability to perform specific bodily functions.
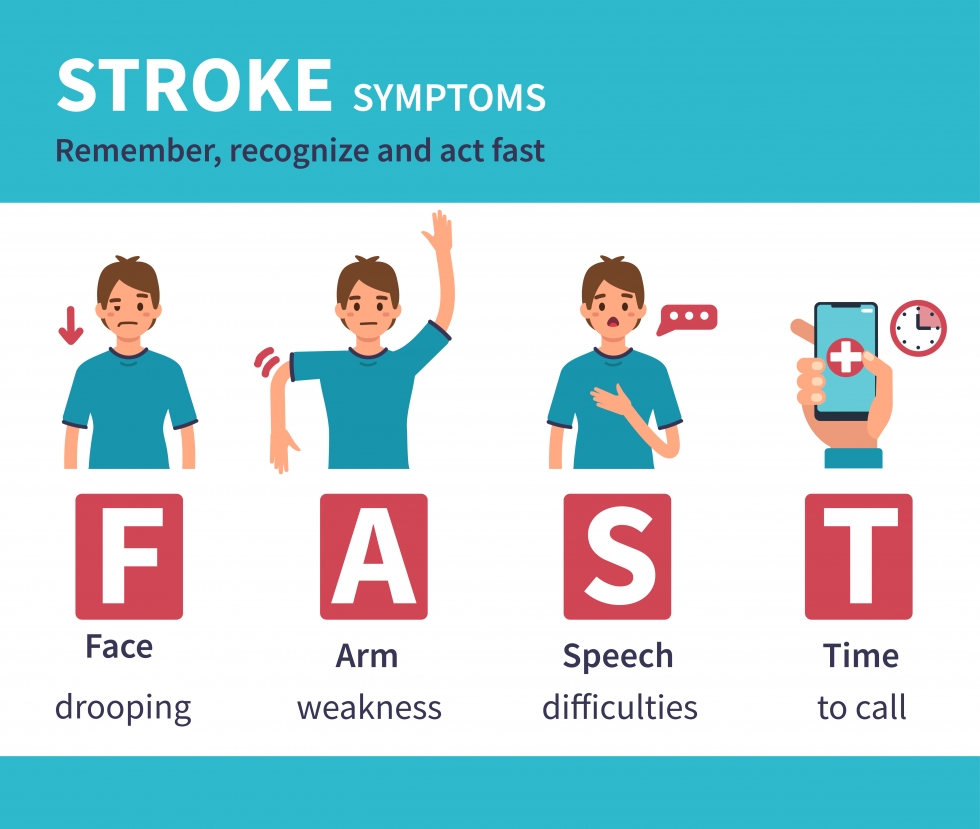
There’s a globally recognized method for identifying stroke symptoms known as the F.A.S.T. test:
- F – Face: Facial drooping or asymmetry, typically on one side.
- A – Arm: Sudden weakness or inability to lift one arm (or leg).
- S – Speech: Slurred, confused, or completely lost speech.
- T – Time: Time is critical. If you notice any of these signs, call emergency services and get the patient to a stroke-ready hospital immediately.
What’s crucial to understand is this: “trúng gió” does not cause paralysis, facial drooping, loss of speech, or significant confusion. Delaying proper treatment in favor of home remedies like scraping or acupressure may cost the patient their best chance at survival and recovery.
If there’s any doubt, always choose the safer path: get the person to a medical facility with neurological care as soon as possible.
If someone shows signs of a stroke, what’s the very first thing we should do? Are there any actions we should avoid?
The most important thing is not to hesitate and absolutely not to attempt treatment at home. Call emergency services immediately. In Vietnam, the 115 Emergency Medical Service has expanded its network of stroke response centers across multiple regions. When you call 115, medical staff will provide guidance and transport the patient to the nearest hospital equipped for stroke intervention.
While waiting for emergency responders to arrive, if you have first-aid training, you can:
- Lay the patient on their side to prevent the tongue from falling back and blocking the airway, especially important if the patient has reduced consciousness.
- Monitor their breathing and circulation, and be prepared to perform CPR if necessary.
Importantly, do not give the patient anything to eat or drink, do not attempt to administer medication, and avoid traditional practices like lemon drops, acupressure, or coin scraping, since these can delay proper care and potentially worsen the outcome.
In stroke treatment, there are several critical time windows often referred to as “golden hours”:
- Within the first 4.5 hours: This is the ideal window for administering clot-busting drugs (thrombolytics), typically used for ischemic strokes caused by blood clots.
- Within 6 hours: This is the optimal time to perform mechanical thrombectomy, using a device to physically remove the clot and restore blood flow.
- Between 6 and 24 hours: This is no longer considered the “golden window,” but intervention may still be possible in select cases. Doctors will carefully assess the patient’s imaging results, the extent of brain injury, and clinical status to decide whether further treatment is appropriate. However, treatment outcomes during this period are generally less favorable compared to interventions within the first 6 hours.
On average, how many stroke cases does the Interventional Neurology Department at UMC handle each day? And how many of those patients arrive within the "golden hour" and successfully receive intervention?
Currently, our department receives between 5 to 10 stroke cases per day, with approximately two-thirds being ischemic strokes and the remainder hemorrhagic strokes. Based on imaging and clinical criteria, about two patients per day typically qualify for emergency intervention.
The encouraging news is that the percentage of patients arriving within the “golden window” has significantly improved in recent years. About a decade ago, only 3% of stroke patients reached us within the first 6 hours. Today, that number has risen to 10-15%, which is a reflection of improvements in emergency response systems, public awareness, and cross-department coordination within the hospital.
Looking ahead, our goal is to increase this rate to 20% in the coming year, with continued efforts in outreach, training, and early detection.
When it comes to stroke treatment, what are the key factors that determine its success?
Stroke intervention is a complex, multi-step process. To ensure the best possible outcomes, there are four key factors that significantly influence the effectiveness of treatment:
First is time - the single most critical factor.
The shorter the time between the onset of symptoms and the start of treatment, the better the prognosis. We estimate that time alone accounts for over 50% of a patient’s chance of successful recovery.
Second is the quality and predictability of the intervention itself.
In clinical practice, we assess the effectiveness of vessel recanalization using TICI scores (Thrombolysis in Cerebral Infarction), ranging from 2A to 3. Patients who achieve TICI 2B or 3, meaning near-complete or complete reperfusion, typically have significantly better clinical outcomes.
Third is seamless coordination across multiple specialties.
Effective stroke care involves the smooth collaboration of departments including emergency medicine, neurology, radiology, pharmacy, rehabilitation, and even psychological support. Each step must work in sync for the entire care pathway to function optimally.
Lastly, post-procedure support and recovery play a vital role.
Many assume treatment ends once the intervention is completed. In reality, the recovery journey can be long and demanding, from physical rehabilitation and speech therapy to emotional and cognitive recovery. Holistic, long-term care is essential for restoring the patient’s quality of life.
As you mentioned earlier, time is critical in stroke treatment. What has your team done to improve speed and efficiency during emergencies?
One of the first and most important steps in stroke treatment is determining whether or not intervention is appropriate. This decision, what we call the clinical indication, requires precise, objective analysis under severe time pressure.
To support that, our team uses RAPID AI, one of the most advanced AI-powered imaging platforms available today. It’s been trained on a vast global dataset of medical imaging, allowing it to analyze brain scans within minutes and deliver insights that align closely with real-world clinical outcomes.
This technology helps us draw a clear line between when intervention is likely to be beneficial and when it may carry more risk than reward. What sets RAPID AI apart is not just its speed, but its proven clinical accuracy, giving physicians the confidence to make time-sensitive decisions that can dramatically impact a patient’s recovery.
Compared to international benchmarks (for example, the standard of administering clot-busting drugs within 60 minutes of hospital arrival), what achievements has your team accomplished in acute stroke care?
We’ve made it a priority to not only meet but exceed international standards in stroke intervention. Here are some of the key performance indicators that we’re proud to consistently maintain:
- Door-to-needle time (from hospital arrival to administration of thrombolytic therapy):
- International standard: under 60 minutes
- At our hospital: averages around 30 minutes
- Door-to-puncture time (from hospital arrival to groin puncture for mechanical thrombectomy):
- International standard: under 90 minutes
- At our hospital: often under 60 minutes, with some cases as fast as under 15 minutes
- Successful reperfusion rate (restoring blood flow after intervention):
- Global average: around 75–80%
- At our hospital: consistently above 90%
- Post-intervention functional recovery rate:
- Currently about 55–60%, which is a very strong outcome by global standards.
These achievements are not only encouraging but have also met the stringent criteria set by the Angels Initiative - a global program focused on improving stroke care. As a result, our hospital has been awarded the Diamond Award, the highest level of recognition, signifying stroke management performance on par with the world’s leading centers.

For individuals who wish to assess their risk of stroke early, what types of screening or evaluations are recommended?
Stroke is often the result of a long, silent process, years of gradual changes in the blood vessels that usually go unnoticed, especially in younger individuals. The good news is, research shows that up to 80% of strokes are preventable, especially when people begin making healthy lifestyle changes early on.
Currently, international guidelines do not recommend routine stroke screening for the general population. Instead, screening should be prioritized for individuals in higher-risk groups, those with a family history of cardiovascular disease, or who, during routine health checkups, show warning signs such as high blood pressure, diabetes, or elevated cholesterol levels.
In select cases, physicians may also recommend a carotid artery ultrasound to detect any signs of atherosclerosis (plaque build-up in the arteries), especially when clinical suspicion is high.
But more than any test, I believe the most important strategy lies in everyday prevention. I understand that many young people today live under constant pressure from work, study, and social demands. Still, a few consistent habits can make a world of difference:
- Quit smoking - or at least begin to cut back. Smoking increases stroke risk by 2–3 times.
- Respect your sleep - quality rest is critical for vascular health.
- Exercise regularly - it doesn’t need to be intense; light, consistent activity is enough.
- Maintain a balanced diet - avoid excess salt, sugar, and deep-fried or processed foods.
And one last thing I strongly encourage: learn basic first aid and CPR. Not only can it help protect your own health, but it might one day save someone else’s life.
Thank you very much, Dr. Trần Quốc Tuấn!
